Abstract
Glanzmann thrombasthenia (GT) is an autosomal recessive bleeding disorder which can result in mild to severe mucocutaneous bleeding. Patients with GT usually have normal platelet count, no clumping noted on peripheral blood smear and distinctly abnormal platelet dysfunction studies. NovoSeven®RT has been approved for treatment of this disease, however some patients have ongoing bleeding in spite of treatment with NovoSeven®RT and platelet transfusions. To add to the complexity of the treatment plan, sometimes the bleeding is retropharyngeal and children swallow blood making a timely assessment even more difficult. This case report summarizes additional tools used to control nasal bleeding and the use of TEG (Haemonetics Corporation) to assess therapeutic interventions.
Our patient is a 6 year old female with GT who has behavioral issues and has lived in numerous foster homes. Severe nasal and retropharyngeal bleeds have resulted in repeated emergent transfusions. Part of the difficulty in her management has been her ability to swallow large amounts of blood without notifying her caregiver. She has had multiple blood transfusions and has had an allergic response to platelet plasma requiring washed platelet products with premedication (Benadryl/Solumedrol/Tylenol). Consideration for unrelated HLA donor stem cell transplant had been explored, however our patient's behavioral issues made her less likely to tolerate the transplant process. Her current treatment plan was developed to address local control, systemic control and to attempt to develop a means of assessing therapeutic interventions.
Both nares and her retropharyngeal region were her primary bleeding sites. ENT evaluation identified numerous telangiectasias (AFP= 0.09). Repeated surveillance and cauterization followed by estrogen cream applied to the nasal mucousa twice daily greatly diminished the number of telangiectasias. Amicar® nasal spray (compounded as 10% nasal spray, used as 0.1 mL spray in each nostril), Zyrtec® nasal spray, nightly use of humidifier, normal saline nose gel, and cellulose gauze are medications used for local prevention and have been effective in preventing minor mouth and nose bleeds from becoming major bleeds.
Systemic prevention regimen consisted of NovoSeven®RT prophylaxis BID 2 mg (90 mcg/kg/dose), Amicar® BID and behavioral support to avoid causing self induced trauma/bleeding. Since starting this regimen, all of her bleeds have been related to trauma or digital manipulation. NovoSeven®RT administered every 2 hours in addition to Amicar® TID and 1 to 2 units of washed pheresis platelets were utilized for treatment of active bleeding.
Because of 2 prolonged bleeding episodes following transfusion with a single washed pheresis platelet unit, we attempted to find testing to assist us with evaluation.
TEG Studies and Interpretation
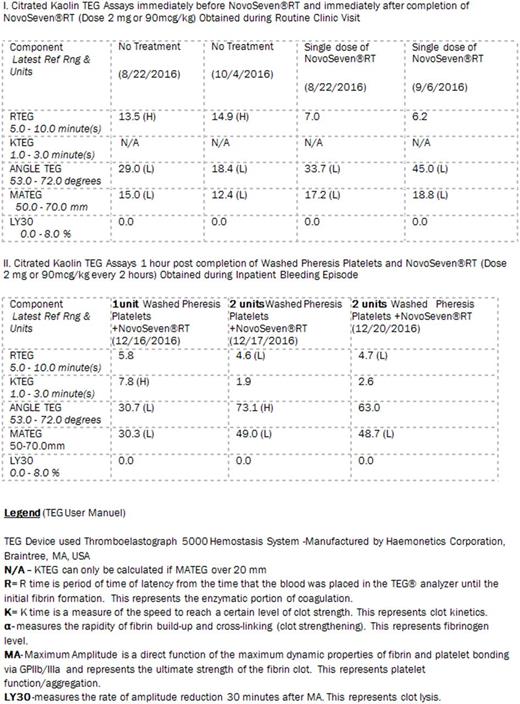
I. Table 1
With a single dose of NovoSeven®RT our patient's RTEG value (time to produce thrombin) improved. However, the rate of clot development/propagation only improved to varying degrees (ANGLE TEG). The overall clot strength (MATEG) remained virtually unchanged.
II. Table 2
With a single washed pheresis unit of platelets, RTEG normalized and MATEG as well as the rate of propagation of the clot improved, however these values were not normal.
With more than one washed pheresis platelet unit and NovoSeven®RT, TEG values almost normalized or returned to normal range, including clot strength represented by MATEG. These findings suggested the greater number of normal platelets transfused increased the likelihood of normal thrombin generation and clot formation. The loss of platelet product from washing likely resulted in decreased platelet numbers, perhaps decreasing the effectiveness of a single washed pheresis unit.
We have utilized these findings to assist with the treatment of severe bleeds and to determine if more washed platelets would be beneficial when clinically the extent of bleeding cannot be determined in a short amount of time (i.e retropharyngeal bleeding). TEG is especially suited for rapid assessment and frequently used in Adult Trauma Centers. Treatment of a pediatric patient with significant bleeding and behavioral concerns requires a tool box of supportive measures. With local, systemic measures and use of TEG, we have been able to improve the safety of our GT patient, with decreases in major bleeds over the last year.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal